Minimally Invasive Rotator Cuff Sparing Shoulder Replacement Surgery
A board-certified, fellowship-trained orthopaedic shoulder surgeon and sports medicine specialist, Dr. Steven Chudik is renowned for his shoulder expertise and innovative procedures that reduce surgical trauma, speed recovery and yield excellent outcomes.
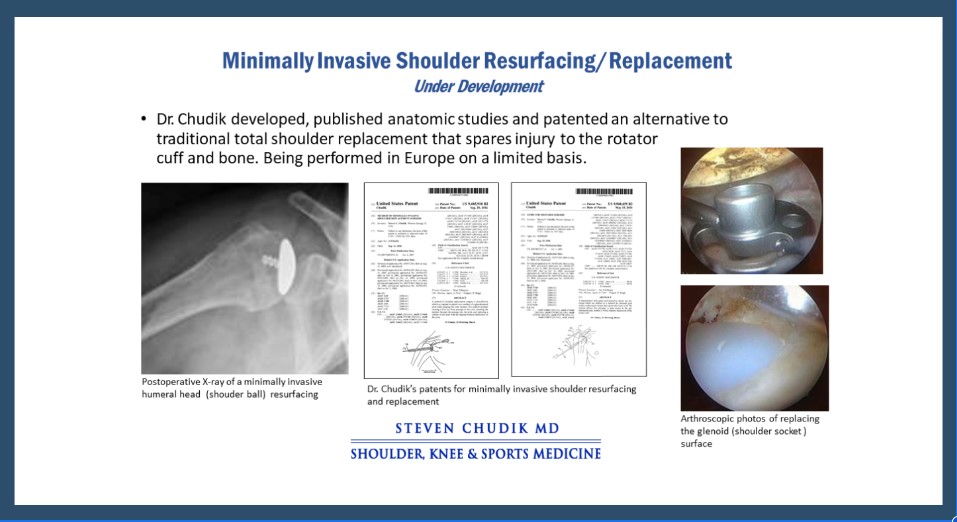
Through his research, Dr. Chudik investigates and pioneers advanced and novel minimally invasive procedures, instruments and implants that have forever changed patients’ lives. Never content to settle for what’s always been done for orthopaedic shoulder care. Dr. Chudik prides himself on providing individualized care and developing a plan that is right for each patient. By taking this approach for the past 20 years, Dr. Chudik has developed minimally invasive surgical techniques and instruments for shoulder replacement surgery. Back in the early 2000’s, Dr. Chudik discovered and patented a minimally invasive total shoulder replacement surgery that spares the rotator cuff and avoids dislocating the shoulder. Traditional shoulder replacement surgery requires cutting the rotator cuff and repairing it and 6 weeks of immobilization in a sling to allow the rotator cuff to heal, and 4-6 months to rehabilitate. Dr. Chudik’s technique avoids damaging the rotator cuff, avoids the sling, and allows the patient to actively move the shoulder immediately following surgery. This avoids permanent damage to the rotator cuff and expedites a full recovery.
Shoulder Replacement Expertise
- Non-operative treatment of shoulder arthritis
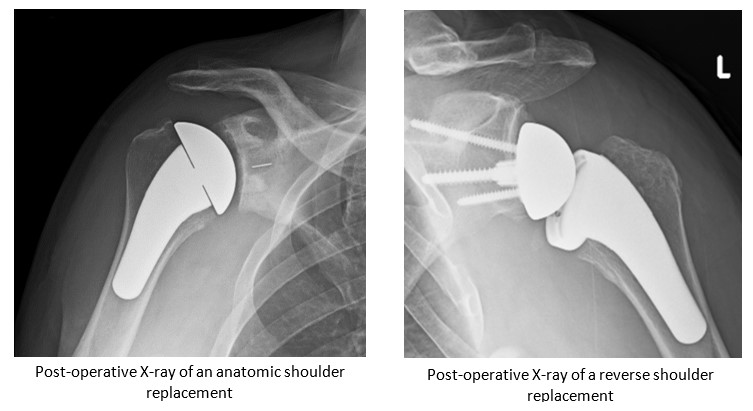
- Total Shoulder Arthroplasty (TSA)
- Reverse Total Shoulder Arthroplasty (RTSA)
- Minimally Invasive (Rotator Cuff Sparing) Shoulder Replacement **Coming Soon**
- Massive rotator Cuff Repair
- Biologic Shoulder Resurfacing for Shoulder Arthritis
Individualized Treatment and Rehabilitation
Because no two people and no two injuries are alike, Dr. Chudik uses his expertise to develop and provide individualized care and recovery plans for his patients. This personal attention explains why patients travel to have Dr. Chudik care for their shoulder conditions and injuries.
Dr. Chudik expects better than average outcomes and provides specific treatment, rehabilitation, and return to activity protocols for golf, throwing, and other overhead sports.
Frequently Asked Questions
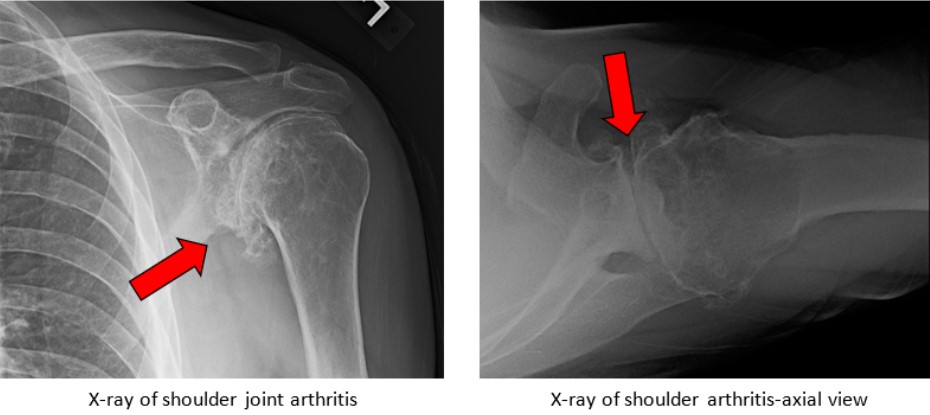
Glenohumeral (shoulder) arthritis occurs when the protective cartilage on the surface of the glenoid (socket of the shoulder joint) and the humeral head (ball of the shoulder joint of the upper arm) wears out. As a result, patients experience shoulder pain, decreased range of motion, decreased strength, and functional limitation as the worn ends of the bones grind together, deform, and cause inflammation.
This cartilage surface breaks down from genetic susceptibility, excessive joint loading over time, systemic disease, or following injury. Previous injury to the glenohumeral joint can damage the cartilage and result in accelerated wearing out of the protective cartilage on the ends of the bones, i.e. arthritis. Heavy and/or repetitive loading of the shoulder joint over prolonged periods of time such as those associated with weightlifting and/or heavy labor can accelerate the arthritis process. Some patients are genetically more susceptible to developing arthritis. Patients with susceptibility may develop arthritis regardless of activity level. Additionally, inflammatory or autoimmune diseases that damage articular cartilage, such as rheumatoid arthritis can cause arthritis.
- Shoulder pain, weakness, and decreased range of motion
- Shoulder pain that worsens with activity
- Shoulder stiffness that is worse in the morning or with a lack of activity
- Pain at night that affects the patient’s ability to sleep due to increased activity during the day
Shoulder (glenohumeral joint) arthritis is diagnosed through a combination of patient history, physical exam and x-ray imaging. Commonly, patients will report a history of previous shoulder injury or surgery, family history of arthritis, or history of autoimmune disease other systemic health issues affecting their joints. Physical exam typically reveals reduced range of motion, pain with motion, and strength deficits. X-ray imaging will often reveal the presence of shoulder (glenohumeral) joint arthritis and the degree of severity as well. Sometimes MRI is also helpful for directly visualizing damaged cartilage.
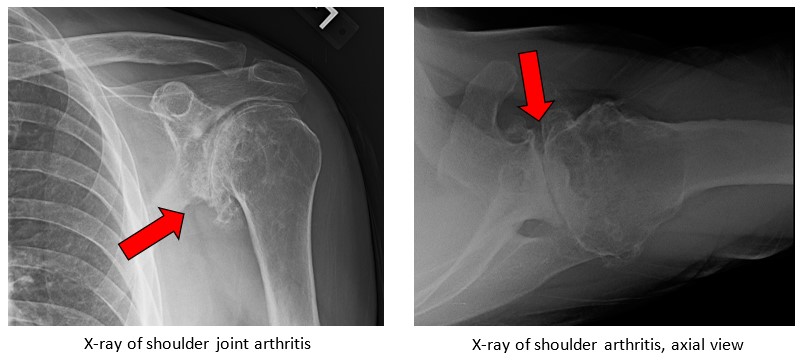
The treatment and outcomes depend upon age, symptoms, severity, deformity, and other associated shoulder pathology like rotator cuff tears. Not all patients with X-ray findings of shoulder (glenohumeral) joint arthritis have pain. Typically, it is the younger, more active patients (who place higher demands on their shoulders) that have more pain. Older, less demanding patients can often expect excellent results by utilizing conservative management.
Initial treatment consists of activity modification (reduce the aggravating activities) as well as rest, ice, and anti-inflammatory medications to relieve pain. Specific physical therapy programs and injections can reduce inflammation and pain and improve motion and function. Shoulder replacement surgery is beneficial when patients continue to have symptoms despite conservative treatment. In rare cases, extreme loss of shoulder motion and erosion (destruction) of the glenoid (socket of the shoulder joint) call for earlier intervention and surgery.
When symptoms warrant, Dr. Chudik can replace the damaged and arthritic joint surfaces of the shoulder. In general, shoulder replacement (total shoulder arthroplasty) surgery is well-tolerated. Shoulders with a compromised or chronically torn and irreparable rotator cuff, severe deformity, or instability may require a reverse shoulder replacement.
- As long as the patient is otherwise healthy, shoulder replacement surgery is performed at an outpatient facility and the patient can safely return home the same day as surgery.
- The surgery is performed under limited general anesthesia and an interscalene nerve block (local anesthetics are used to numb the entire shoulder and arm for up to 12-24 hours after surgery).
- During traditional techniques of shoulder replacement surgery, the rotator cuff needs to be cut for proper exposure and then repaired which requires the patient to wear a sling and not use arm for 6 weeks following surgery.
- The patient is not allowed to actively move their shoulder with their own shoulder muscles for at least six weeks following surgery in order to protect the rotator cuff and allow it to heal.
- It may feel more comfortable sleeping sitting upright on a couch, recliner chair, or propped up in bed after surgery.
- It is important to keep the wound clean and dry for 10 to 14 days following open shoulder surgery. Showering lightly after 14 days is fine but wounds cannot be submerged under water until three weeks after surgery.
- Driving is typically acceptable at 6 to 8 weeks after surgery. Physical therapy should begin two to three days after surgery and continue for four months. The success of a shoulder replacement surgery is highly dependent on the post-operative rehabilitation. It is crucial to follow through and maintain a proper therapy schedule.
- The patient may return to sedentary work in less than one to two weeks as long as they are in their sling and do not use the involved extremity.
- No typing, writing, or purposeful movement of that arm is allowed for the first six weeks following surgery.
- The patient may return to their previous recreational activities when their rehabilitation is complete and functional use has been restored.
- Usually, four to six months is necessary to restore range of motion and strength and allow a safe return to activities. Dr. Chudik has specialized programs for returning to activities such as golf that will be discussed at the patient follow-up appointments.
The goal of shoulder replacement surgery is to relieve the patient’s pain from shoulder (glenohumeral) joint arthritis. Returning to strenuous repetitive and heavy lifting activities is not advised following shoulder replacement surgery and places the hardware components in the shoulder at risk for loosening and failure. It is reasonable to expect to return to a recreational active lifestyle following the successful shoulder replacement surgery.
Testimonials and Patient Stories
Shoulder Anatomy
The shoulder possesses a remarkable range of motion, making it one of the most mobile and important joints in your body. Whether you are throwing a baseball, working overhead or performing everyday tasks of reaching and carrying, your shoulder motion is critical to this high level of function. Unfortunately, this increased mobility and structural complexity makes your shoulders susceptible to injuries that can be quite limiting and disabling.
The shoulder consists of three bones, three main joints and an articulation between the scapula (shoulder blade) and thorax (chest):
Scapula (shoulder blade)
Clavicle (collar bone)
Humerus (upper arm bone)
Glenohumeral joint (shoulder joint)
Acromioclavicular joint (shoulder blade-collar bone joint)
Sternoclavicular joint (sternum-collar bone joint)
Scapulothoracic articulation (shoulder blade-chest connection)
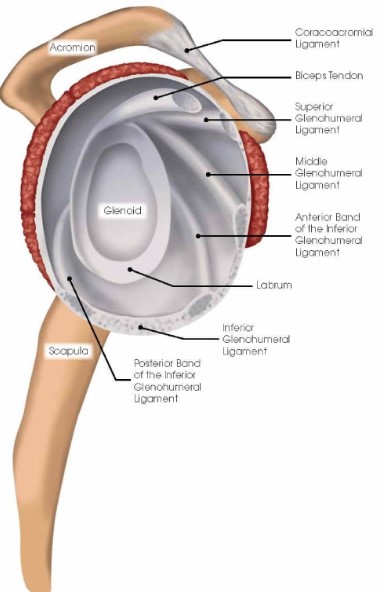
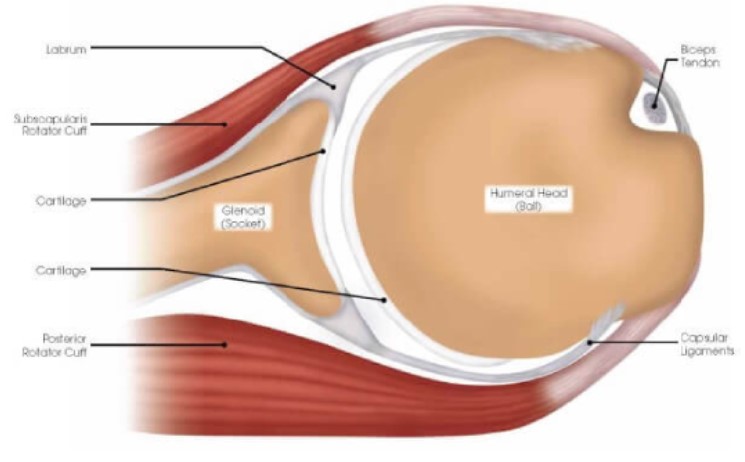
Labrum and Ligament Anatomy
The shoulder has a labrum or thickening of firm soft-tissue attached to the rim of the glenoid (socket). It deepens the socket to increase stability, bears load and serves as the attachment point for ligaments that run between the upper arm bone and the bony glenoid (socket).
Ligaments are strong soft-tissue bands that connect bones at a joint, provide stability and proper limits to motion. The labrum and ligaments may be torn if forces cause the humeral head (ball) to abruptly shift from the glenoid (socket) such as during a shoulder dislocation. Shoulder ligaments get their names from the bones to which they connect and include the superior glenohumeral ligament (SGHL), middle glenohumeral ligament (MGHL) and the inferior glenohumeral ligament (IGHL) with important anterior and posterior bands. There also are other important ligaments in the shoulder including the acromioclavicular, coracoclavicular and the sternoclavicular ligaments.
Cartilage
The joint surfaces of the shoulder are covered with a thin, but durable, layer of cartilage over the ends of the humeral head (ball) and glenoid (socket) that allows the shoulder surfaces to articulate, move smoothly—almost frictionless and painlessly along each other. The cartilage lacks a blood supply. It gets nutrition from joint fluid. Without a blood supplyand because of its relatively less active cellular makeup, cartilage cannot maintain or repair itself. The cartilage is extremely durable, but in time with “wear and tear” or following injury, it breaks down, fails, and leads to cartilage damage and eventually symptomatic (pain, stiffness, swelling) arthritis (failure of this protective joint surface).
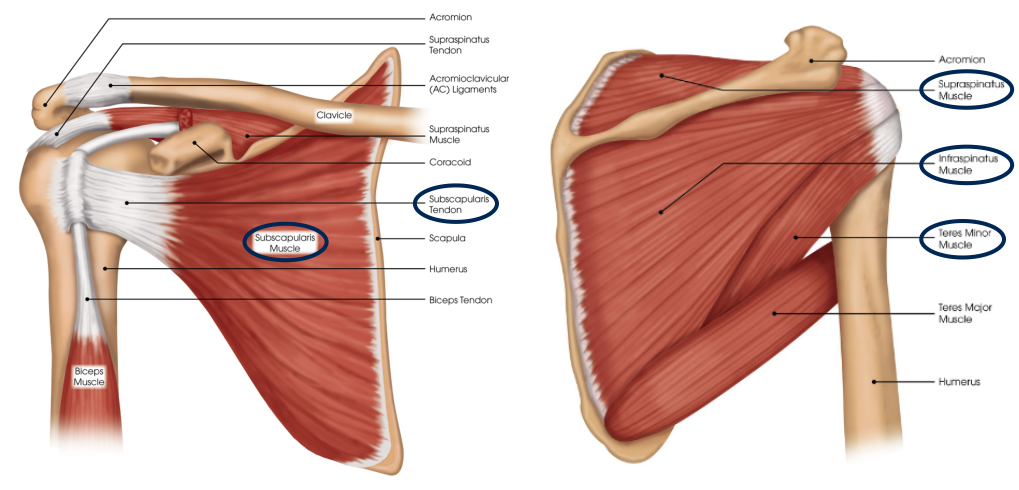
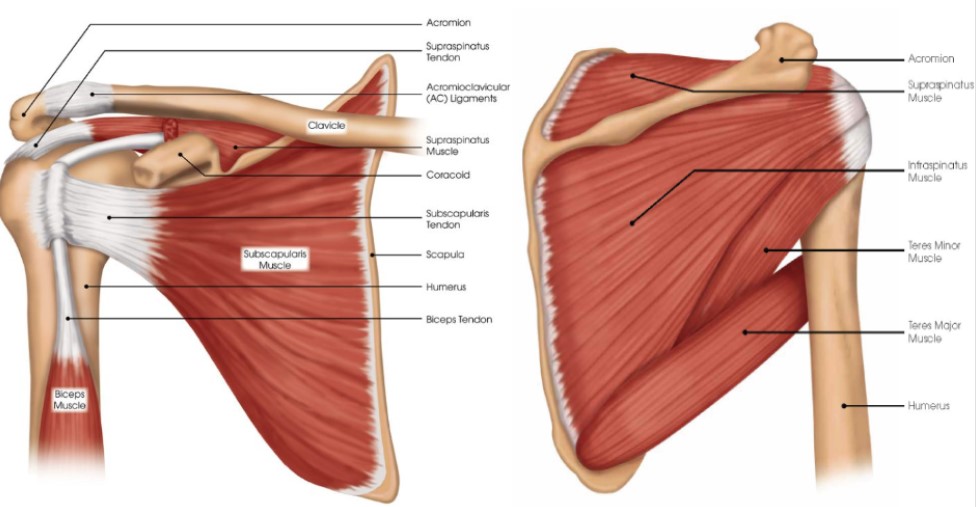
Muscles
The shoulder has several muscles that help it move with proper coordination and strength to accomplish tasks ranging from simple reaching to high level overhead athletic maneuvers. Muscles are like loaded active springs. They attach to bones across joints by different shaped rope- or band-like tendons to exert their action and cause movement. The rotator cuff is a deep, core group of four muscles. They keep the humeral head (ball) centered on the glenoid (socket) while the pectoralis major, deltoid and latissimus dorsi (the big muscle movers of the arm) create pulling and pushing forces that would otherwise shift the humeral head out of the glenoid (socket). Even with simple reaching—out and away from your body—the rotator cuff must generate forces equal to almost 80 percent of your body weight to keep the humeral head centered in the glenoid. Still greater forces are needed during overhead throwing or strenuous lifting movements. These tremendous forces can cause tears in the tendon portion of the rotator cuff and result in pain and arm/shoulder limitations. The long head of the biceps muscle that attaches to the top of the glenoid through the superior (top) labrum also can be injured and cause pain. Additionally, muscles control the scapula (shoulder blade) or base of the shoulder joint which can be affected by injury and overuse producing shoulder pain and limitations.
Injuries and Conditions
Surgical Procedures
- Total Shoulder Arthroplasty
- Reverse Total Shoulder Arthroplasty
- Arthroscopic Biologic Total Shoulder Resurfacing (Developed by Dr. Chudik
- Minimally Invasive (Rotator Cuff Sparing) Shoulder Replacement **Coming Soon**

About Dr. Chudik

- Curriculum Vitae (CV)
- Video
- Website: stevenchudikmd.com
- Schedule an appointment online
- Email: contactus@chudikmd.com
- Phone: 630-324-0402
Innovations
Through his research, Dr. Chudik investigates and pioneers advanced and novel arthroscopic procedures, instruments and implants that change patients’ lives because of better long-term outcomes, or outcomes that were never possible previously. His efforts continue to yield scores of patents that will positively affect orthopaedic surgical techniques worldwide.
Novel Procedures
- Arthroscopic Total Shoulder Resurfacing (Under Development)
- Minimally Invasive (Rotator Cuff Sparing) Shoulder Replacement **Coming Soon**
US Patents and Patent Applications
Dr. Steven Chudik continually innovates to create new technology, surgical techniques and improve patient care. He also collaborates worldwide with other leaders in the orthopaedic technology industry. Surgeries provide Dr. Chudik with an endless source of ideas to create new, safer, less invasive, and more effective surgical procedures, surgical instruments and implants. Several of his shoulder patents are the direct result of these pioneering endeavors.
-
-
- Method of Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,445,910, filed September 11, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery. Patent application serial number 11/529,185 case II, filed September 25, 2006
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,974,658, filed September 25, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery, Serial No.11/525,629, filed September 25, 2006, application published as U.S. Patent App. Pub. 2007/0016305 (A)
- Guide for Shoulder Surgery, U.S. Patent No. 9,968,459, filed September 29, 2006
- Suture Pin Device. Patent application serial number 11/529,2006, case XV, filed September 29, 2006
- Suture Pin Device, Serial No. 11/529,185, filed September 29, 2006, application published as U.S. Patent App. Pub. 2007/0027477 (A)
-
-
-
- Method of Arthroscopic or Open Rotator Cuff Repair Using An Insertional Guide For Delivering a Suture Pin, U.S. Patent No. 8,540,737, filed October 24, 2006
- Acromioclavicular Joint Repair System, U.S. Patent No. 9,387,011, filed February 2, 2007
- Resurfacing Implant for a Humeral Head, Serial No. 13/068,309, filed May 9, 2011, application published as U.S. Patent App. Pub. 2012/0041563 (A)
- Universal Anterior Cruciate Ligament Repair and Reconstruction System(Cannulated Scalpel), U.S. Patent No. 10,034,674, filed February 2, 2007
- Resurfacing Implant for a Humeral Head. Patent application serial number 13/068,309 case II (A), filed May 9, 2011
- Method of Arthroscopic or Open Rotator Cuff Repair Using an Insertional Guide for Delivering a Suture Pin. U.S. Patent Number 8,540,737 B2, issued September 24, 2013
- Cortical Loop Fixation System for Ligament and Tendon Reconstruction, Serial No. 13/998,567, filed November 12, 2013, application published as U.S. Patent App. Pub. 2015/0134060 (A)
- Acromioclavicular Joint Repair System. U.S. Patent Number 9,387,011 B2, issued July 12, 2016
- Method of Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,445,910 B2, issued September 20, 2016
- Guide for Shoulder Surgery. U.S. Patent Number 9,968,459 B2, issued May 15, 2018
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,974,658 B2, issued May 22, 2018
- Glenoid Implant with Replaceable Articulating Portion, U.S. Patent No. 11,406,505, filed August 20, 2019, issued August 9, 2022
- Cortical Loop Fixation Method for Ligament and Bone Reconstruction, Serial No. 15/731,719, filed July 24, 2017, application published as U.S. Patent App. Pub. 2019/0021845 (Pending)
- Humeral Implant and Method, Serial No. 17/532,714, filed November 22, 2021 (Pending), published as U.S. Patent App. Pub. US 2023/0157832
- Humeral Implant with Cannulation and Method, Serial No. 18/211,396, filed June 19, 2023 (Pending)
- Glenoid implant with Portal and Method, filed July 2023 (Pending)
-
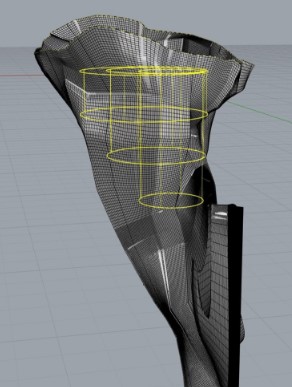
Research
An inquisitive nature was the impetus for Dr. Steven Chudik’s career as a fellowship-trained and board-certified orthopaedic surgeon, sports medicine physician, and arthroscopic pioneer for shoulder injuries. It also led him to design and patent special arthroscopic surgical procedures and instruments and create the Orthopaedic Surgery and Sports Medicine Teaching and Research Foundation (OTRF). Through OTRF, Dr. Chudik conducts unbiased orthopaedic research and provides up-to-date medical information to help prevent sports injuries. He also shares his expertise and passion for mentoring medical students in an honors research program and serving as a consultant and advisor for other orthopaedic physicians and industry.
Areas of Shoulder Research And Development
- Shoulder Replacement
- Rotator Cuff Repair
- Shoulder Instability and Dislocations
- Acromioclavicular Injuries
- Shoulder Fractures
- Shoulder Anesthesia
- Throwing Shoulder and Elbow Injuries